Losing a limb can significantly impact an individual’s ability to interact with their environment. For individuals with lower-limb amputation, the loss of agency in their limbs can make it challenging to navigate everyday situations.
Prosthetic devices are often used to help amputees relearn how to move around, but these devices are often mechanically passive with a predetermined stiffness designed primarily for storing and returning energy. Amputee daily life, however, contains many activities that require active generation of energy at the missing limb, and their prosthetic device provides no active support during these tasks.
According to a new study from North Carolina State University and the University of North Carolina at Chapel Hill, robotic prosthetic ankles that are controlled by nerve impulses allow amputees to move more “naturally,” improving their stability.
“This work focused on ‘postural control,’ which is surprisingly complicated,” says Helen Huang, corresponding author of the study.
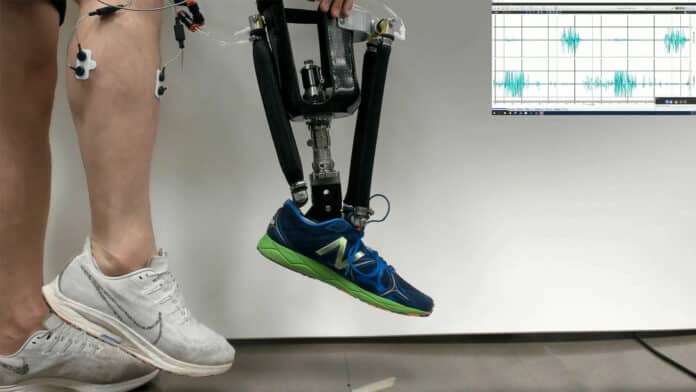
Researchers have developed robotic prosthetic ankles that boost the postural control of the wearer and stability of the lower limb. The robotic prosthetics are controlled using electromyographic (EMG) signals, which are the electrical signals recorded from an individual’s muscles.
They developed their model on a previous work, which demonstrated how a neural-controlled powered prosthetic ankle can restore a range of abilities, including standing on challenging surfaces and squatting.
Electromyographic sensors on the calf capture electrical activity generated by muscles when they are flexed. This signal tells the prosthesis which artificial muscle to flex and how much to flex. For individuals with amputation, these sensors are placed in the prosthetic socket.
In the new study, researchers worked with five people who had amputations below the knee on one leg. The participants were fitted with a prototype robotic prosthetic ankle that responds to EMG signals detected by sensors on the leg.
“Basically, the sensors are placed over the muscles at the site of the amputation,” says Aaron Fleming, co-author of the study and recent Ph.D. graduate from NC State. “When a study participant thinks about moving the amputated limb, this sends electrical signals through the residual muscle in the lower limb. The sensors pick these signals up through the skin and translate those signals into commands for the prosthetic device.”
The researchers conducted general training for study participants using the prototype device so that they were somewhat familiar with the technology.
The participants were then tasked with responding to an “expected perturbation,” which is something that could affect their balance. To replicate the conditions precisely throughout the study, the researchers created a mechanical system that tested the stability of the participants.
Study participants were asked to respond to the expected perturbation under two conditions: using the prosthetic devices they normally used and using the robotic prosthetic prototype. Researchers found that study participants were significantly more stable when using the robotic prototype and were less likely to stumble or fall.
“Specifically, the robotic prototype allowed study participants to change their postural control strategy,” says Huang. “For people who have their intact lower limb, postural stability starts at the ankle. People who have lost their lower limb normally have to compensate for lacking control of the ankle. We found that using the robotic ankle that responds to EMG signals allows users to return to their instinctive response for maintaining stability.”
In another experiment, researchers instructed the participants to sway back and forth while wearing either their normal prosthetic or the prototype robotic prosthetic. The participants were equipped with sensors designed to measure muscle activity across the entire lower body.
“We found that muscle activity patterns in the lower body were very different when people used the two different prostheses,” Huang says. “Basically, muscle activation patterns when using the prototype prosthetic were very similar to the patterns we see in people who have full use of two intact lower limbs. That tells us that the prototype we developed mimics the body’s behavior closely enough to allow people’s ‘normal’ neural patterns to return. This is important because it suggests that the technology will be somewhat intuitive for users.
“We think this is a clinically significant finding because postural stability is an important issue for people who use prosthetic devices. We’re now conducting a larger trial with more people to both demonstrate the effects of the technology and identify which individuals may benefit most.”