Researchers at Australia’s national science agency, CSIRO, have developed a technique that addresses the challenges of transporting temperature-dependent vaccines. Researchers hope that this may increase access in rural and remote communities in Australia and developing countries.
The CSIRO researchers encapsulated live virus vaccine with a porous, dissolvable, crystalline material called MOFs (metal-organic frameworks), which protected the integrity of the vaccines for up to three months and at temperatures as high as 37 degrees Celsius. Without refrigeration, a vaccine would otherwise last only for a few days.
“Vaccination is undoubtedly one of the most effective medical interventions, saving millions of lives each year, however delivering vaccines, particularly to developing countries, is challenging because they often lack the cold storage supply chains required to keep the vaccine viable,” Dr. Daniel Layton said.
The World Health Organization estimates that up to 50% of vaccines are wasted globally every year, a large part because of lack of temperature control and the logistics to support an unbroken cold chain. Most vaccines need to be kept within the temperature range between +2 °C and +8 °C in order to prevent them from degradation.
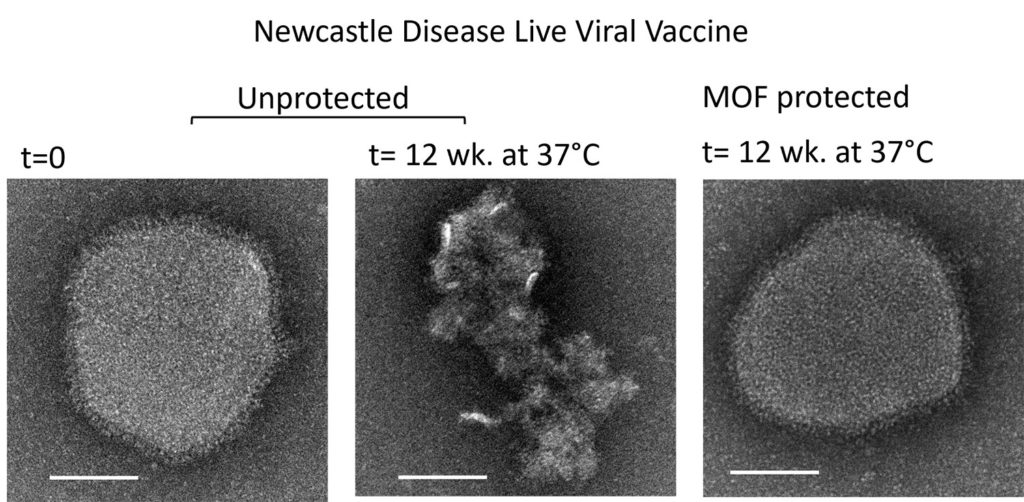
To test their new technique, the researchers focused on two different types of live viruses as proofs of concept, a Newcastle Disease vaccine designed to protect poultry and a strain of Influenza A. The crystalline material coats the vaccine to protect the vaccine molecules from heat stress until the vaccine needs to be administered.
Researchers say MOFs were the perfect material for protecting vaccines from temperature variations. “MOFs are a porous crystalline material that can grow around the vaccine to form a scaffold that protects against temperature variations,” said Dr. CSIRO senior scientist Dr. Cara Doherty. “MOFs work similarly to a scaffold you might put around your house; once you remove the scaffold, your house remains – which is what happens when we dissolve the MOFs in a vaccine.”
“Live virus vaccines are extremely effective, but their complex composition makes them susceptible to high temperatures, and a universal stabilization technique has not been found,” Dr. Layton said. “This breakthrough has the potential to enable more affordable and equitable access to vaccines across the world.”
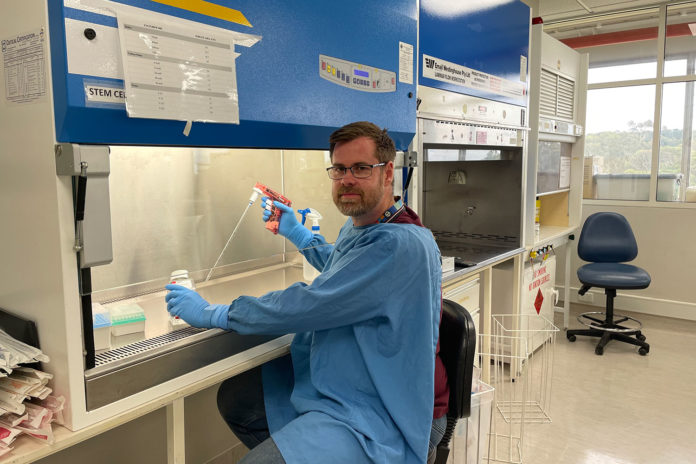
CSIRO researcher and the lead author of the paper, Dr. Ruhani Singh, said their technique is cost-effective and easily scalable, meaning it can swiftly slip into current vaccine manufacturing processes. “This world-first approach of stabilizing a vaccine with MOFs is simple, rapid, and scalable because it takes one step.”
The team continues to progress this research and is looking to partner with animal and human health companies to commercialize their work.